What is gastric bypass?
This surgical procedure is performed in two parts of the digestive system, the stomach, and the small intestine. This surgical technique is conducted under general anesthesia using laparoscopy through four or five small incisions in the abdomen, resulting in less postoperative pain and a rapid recovery.
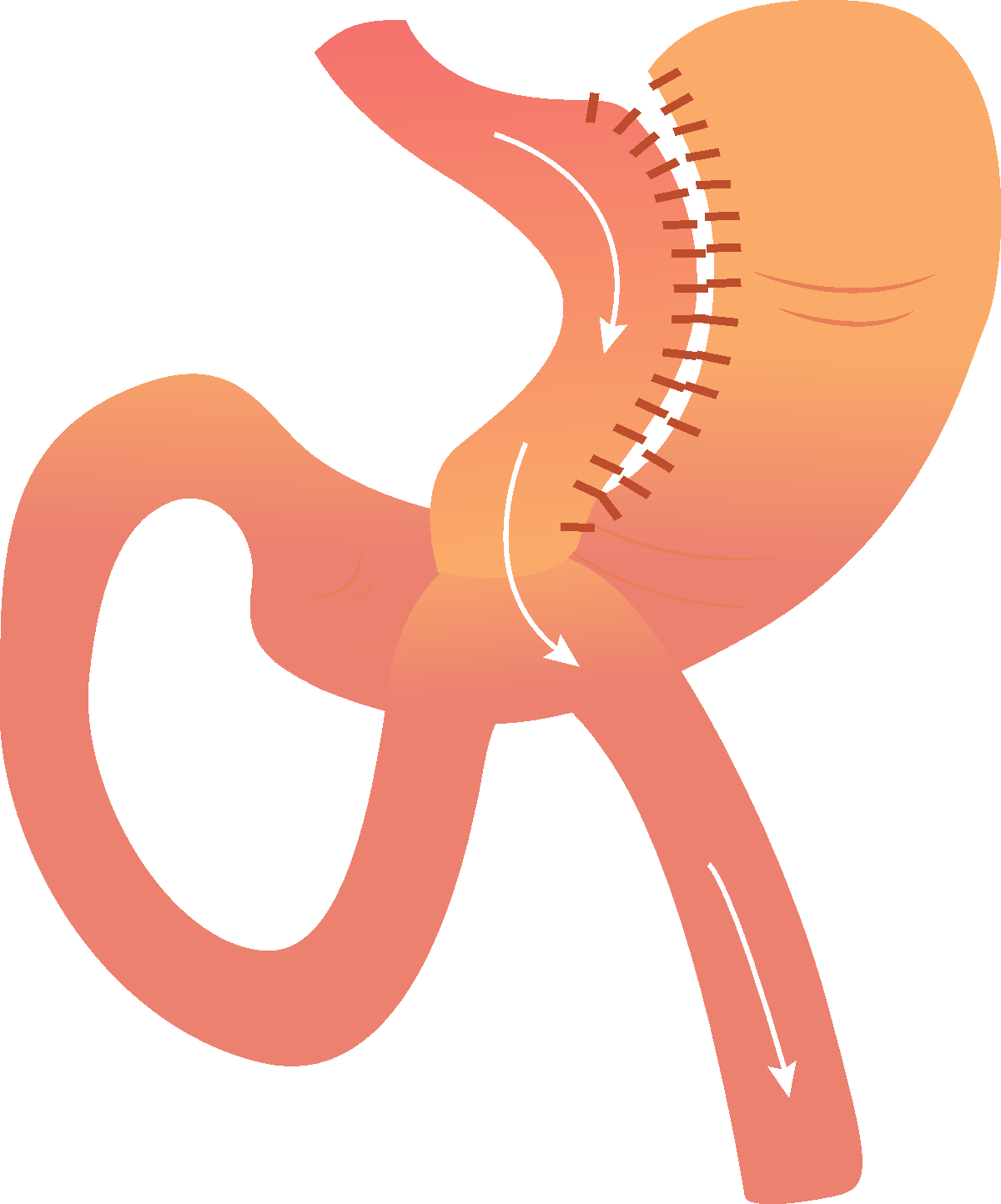
The surgery is divided into two stages


The most commonly practiced gastric bypass technique is called Roux-en-Y gastric bypass.
Given the advances in medicine and the large number of cases operated on worldwide, this technique can be adapted according to the weight reduction needs and associated pathologies of each patient. The adaptation involves varying the size of the stomach and the connection between the stomach and the small intestine.
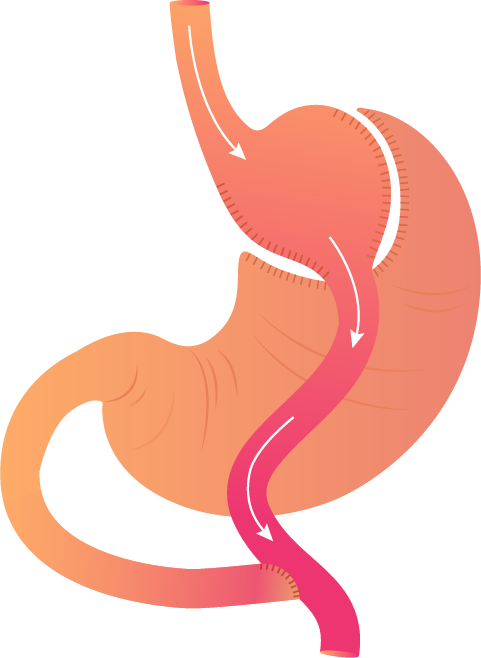
Another variation of the technique used is the single-anastomosis gastric bypass.
This involves creating a stomach that is longer than a conventional bypass, and instead of cutting the intestine, only connecting it to the elongated stomach. This saves an intestinal suture, simplifying the surgery compared to traditional gastric bypass. While technically simpler than the classic gastric bypass, it is associated with a higher component of malabsorption. Therefore, it is recommended for patients with high body mass indexes and/or metabolic diseases associated with obesity.
Another variation of the technique used is the single-anastomosis gastric bypass.
This involves creating a stomach that is longer than a conventional bypass, and instead of cutting the intestine, only connecting it to the elongated stomach. This saves an intestinal suture, simplifying the surgery compared to traditional gastric bypass. While technically simpler than the classic gastric bypass, it is associated with a higher component of malabsorption. Therefore, it is recommended for patients with high body mass indexes and/or metabolic diseases associated with obesity.
The recovery from bariatric surgery is quite rapid and straightforward. On the day of the surgery, immediately after the procedure, the patient can walk and start oral intake with a liquid diet.
In the case of gastric bypass, the patient stays hospitalized for two nights and is discharged on the second day. As part of the postoperative protocol, an intra-abdominal drainage is placed to diagnose bleeding or internal scarring early. It is removed on an outpatient basis between the 5th and 6th days postoperatively.
For this type of surgery, no special care is required, only the following recommendations: washing the wounds with water and soap, avoiding activities involving force, staying active at home, and strictly following the nutritional recommendations provided by the nutrition team.
Between the fourth and fifth days after surgery, the patient can return to their city of origin (for non-residents in the city of Cartagena) or resume their daily activities, including work, except for tasks involving physical exertion.
The patient is discharged with three medications: analgesics, antacids, and an anticoagulant. All patients require protein, vitamin, and mineral supplements for life to maintain the patient in nutritionally healthy conditions.
Regarding physical activity and sports, it is recommended to start brisk walks of one hour five times a week at fifteen days. At thirty days, resistance and strength exercises should be initiated. Regarding the diet, it starts immediately after surgery with clear liquids for three days, followed by a liquid diet for an additional week, and a soft diet for an approximate period of ten days. It is estimated that around the fortieth day, the patient can consume solid food, guided by the nutrition team.
What are the complications of Gastric Bypass?
The complications of gastric bypass are very rare. Patients may experience intra-abdominal or abdominal wall bleeding or infection, gastric fistulas, or strictures.
They may also develop pulmonary embolism, blood clots in the blood vessels of the lower or abdominal extremities, mucus plug in the lungs, allergies, and so on. All these complications can be prevented by applying clear protocols for bariatric patient management, performing surgery in optimal clinics, and having it done by specialized surgeons.